Following the implementation of the HPV vaccine immunization programs, real-world studies have further demonstrated that introducing HPV vaccine into the immunization programs is effective in reducing the prevalence of selected high-risk HPV infections, the prevalence of genital warts, cervical epitheliomas, and the incidence of cervical cancer.
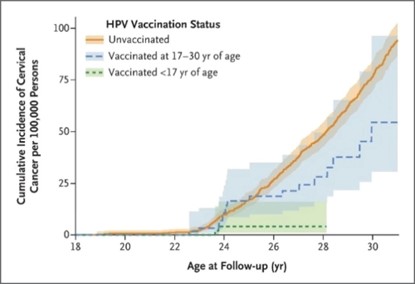
One study reviewing health registry and demographic data from 1.7 million Swedish women aged 10-30 years showed that at least one dose of quadrivalent HPV vaccine significantly reduced the risk of invasive cervical cancer. The benefit was more pronounced in women vaccinated before 17 years old, with a reduction in the incidence of invasive cervical cancer of up to 88% [1] (Figure 1).
Figure 1. Cumulative Incidence of Invasive Cervical Cancer According to HPV Vaccination Status
A systematic review and meta-analysis examined studies evaluating the real-world effects of HPV vaccine promotion in populations between 2014-2018 [2]. The study, covering 65 studies in high-income countries, found that after 5-8 years of vaccine program rollout, the prevalence of high-risk HPV16/18 infections was significantly reduced by 83% in women aged 13-19 years (RR: 0.17, 95% CI: 0.11-0.25) and by 66% in women aged 20-24 years (RR: 0.34, 95% CI: 0.23- 0.49).
The prevalence of HPV31/33/45 infection was reduced by 54% in females aged 13-19 years (RR: 0.46, 95% CI: 0.33-0.66), and the prevalence of diagnosed anal condyloma acuminatum was reduced by 67% in females aged 13-19 years, 54% in females aged 20-24 years, 31% in females aged 25-29 years, and 48% in males aged 15-19 years, and 32% in males aged 20-24 years.
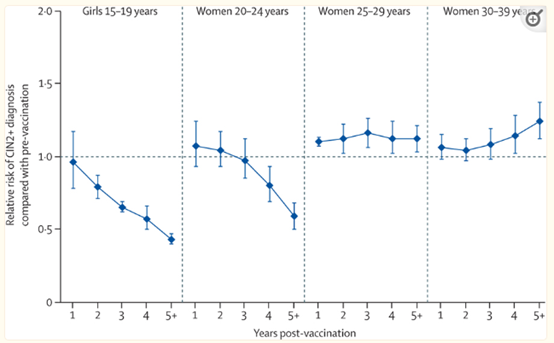
Over the 5-9 years after HPV vaccination, the prevalence of infection with cervical intraepithelial neoplasia grade 2 or 3 was reduced by 51% in screened women aged 15-19 years and 31% in women aged 20-24. Figure 2 reflects the trend in the relative proportion of men and women at risk for anogenital acromegaly and CIN2+ infection over the 8 years after the introduction of HPV vaccines among women, compared with the vaccination program pre-launch period. This further confirms that vaccination at a younger age and with a higher coverage are more effective in reducing disease burden and achieving a protective effect at the population level.
Figure 2A. Changes in anogenital wart diagnoses during the 8 years after the introduction of girls-only human papillomavirus vaccination in countries using the quadrivalent vaccine
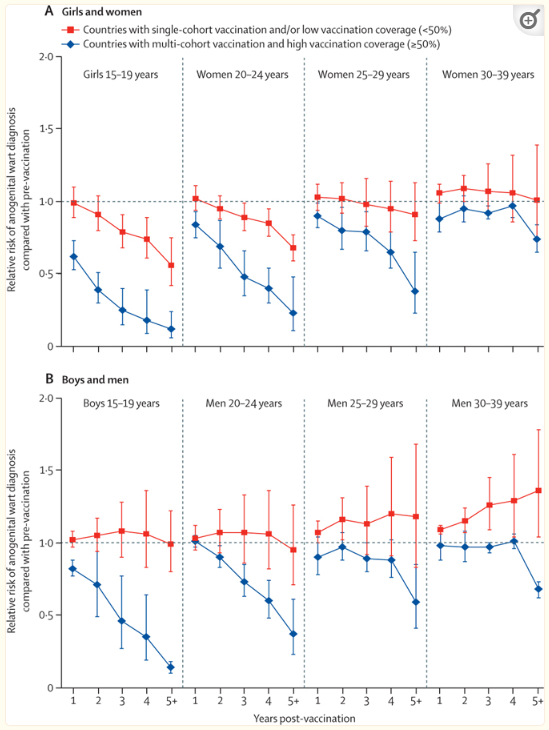
Figure 2B: Changes in CIN2+ among screened girls and women during the first 7 years after the introduction of girls-only human papillomavirus vaccination, in countries with multi-cohort vaccination and high vaccination coverage
Content Reviewer: Kelly Hunter, Tianyi Deng
Page Editor: Jiaqi Zu
References:
- Lei J, Ploner A, Elfström KM, Wang J, Roth A, Fang F, Sundström K, Dillner J, Sparén P: HPV vaccination and the risk of invasive cervical cancer. New England Journal of Medicine 2020, 383(14):1340-1348.
- Drolet M, Bénard É, Pérez N, Brisson M, Ali H, Boily M-C, Baldo V, Brassard P, Brotherton JML, Callander D et al: Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. The Lancet 2019, 394(10197):497-509.





