A study conducted in 2008 shows that pneumonia is the leading cause of death among children under the age of five; more than half of the global pneumonia cases are concentrated in six countries, namely India (43 million), China (21 million), and Pakistan (10 million), as well as Bangladesh, Indonesia, and Nigeria (each with 6 million) (Figures 1, Tables 1 and 2).1 Furthermore, the primary causative pathogen of childhood pneumonia is Streptococcus pneumoniae, accounting for 30-50% of diagnosed cases of pneumonia.1 A global systematic review on the incidence and mortality of pneumonia in children under the age of five showed that the incidence rate in developing countries decreased from 329 per 1000 in 2000 to 231 per 1000 in 2015, and the mortality rate decreased from 15.2 per 1000 in 2000 to 7.4 per 1000 in 2015.2 Additionally, the study found that pneumonia cases in children under the age of five in India, Nigeria, Indonesia, Pakistan, and China exceeded 54% of the global caseload in 2015.
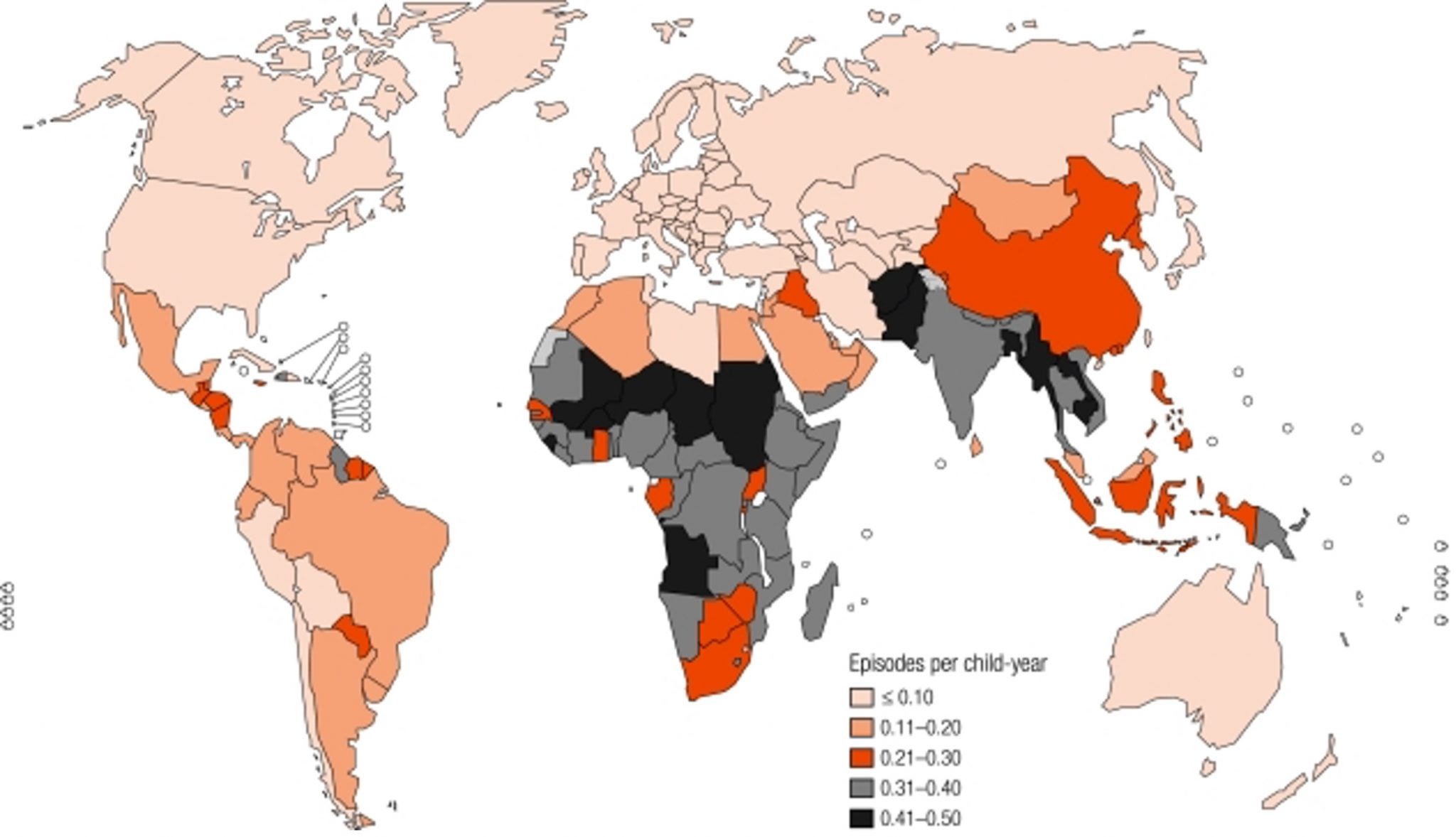
(Source: Rudan I, Boschi-Pinto C, Biloglav Z, et al. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86(5):408-416.)
Table 1 Estimated incidence and number of new cases of pneumonia in children under 5 years of age per year (by WHO organizational region)
| Regions | Total number of children <5 years (millions) | Incidence rate in children (per person-year) | Number of new cases (millions) |
| Africa | 105.62 | 0.33 | 35.13 |
| America | 75.78 | 0.10 | 7.84 |
| Mediterranean region | 69.77 | 0.28 | 19.67 |
| European | 51.96 | 0.06 | 3.03 |
| Southeast Asia | 168.74 | 0.36 | 60.95 |
| The Western pacific region | 133.05 | 0.22 | 29.07 |
| Developing country | 523.31 | 0.29 | 151.76 |
| Developed country | 81.61 | 0.05 | 4.08 |
| Total | 604.93 | 0.26 | 155.84 |
Table 2 Top 15 countries with the highest estimated number of new cases of pneumonia globally, 2008
| Nations | Estimated number of new cases (millions) | Incidence rate in children (per person-year) |
| India | 43.0 | 0.37 |
| China | 21.1 | 0.22 |
| Pakistan | 9.8 | 0.41 |
| Bangladesh | 6.4 | 0.41 |
| Nigeria | 6.1 | 0.34 |
| Indonesia | 6.0 | 0.28 |
| Ethiopia | 3.9 | 0.35 |
| Democratic Republic of the Congo | 3.9 | 0.39 |
| Vietnam | 2.9 | 0.35 |
| Philippine | 2.7 | 0.27 |
| Sudan (ruler of some Muslim states, esp. Ottoman Emperor) | 2.0 | 0.48 |
| Afghanistan | 2.0 | 0.45 |
| Tanzania | 1.9 | 0.33 |
| Myanmar (or Burma) | 1.8 | 0.43 |
| Brazil | 1.8 | 0.11 |
(Source: Rudan I, Boschi-Pinto C, Biloglav Z, et al. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86(5):408-416.)
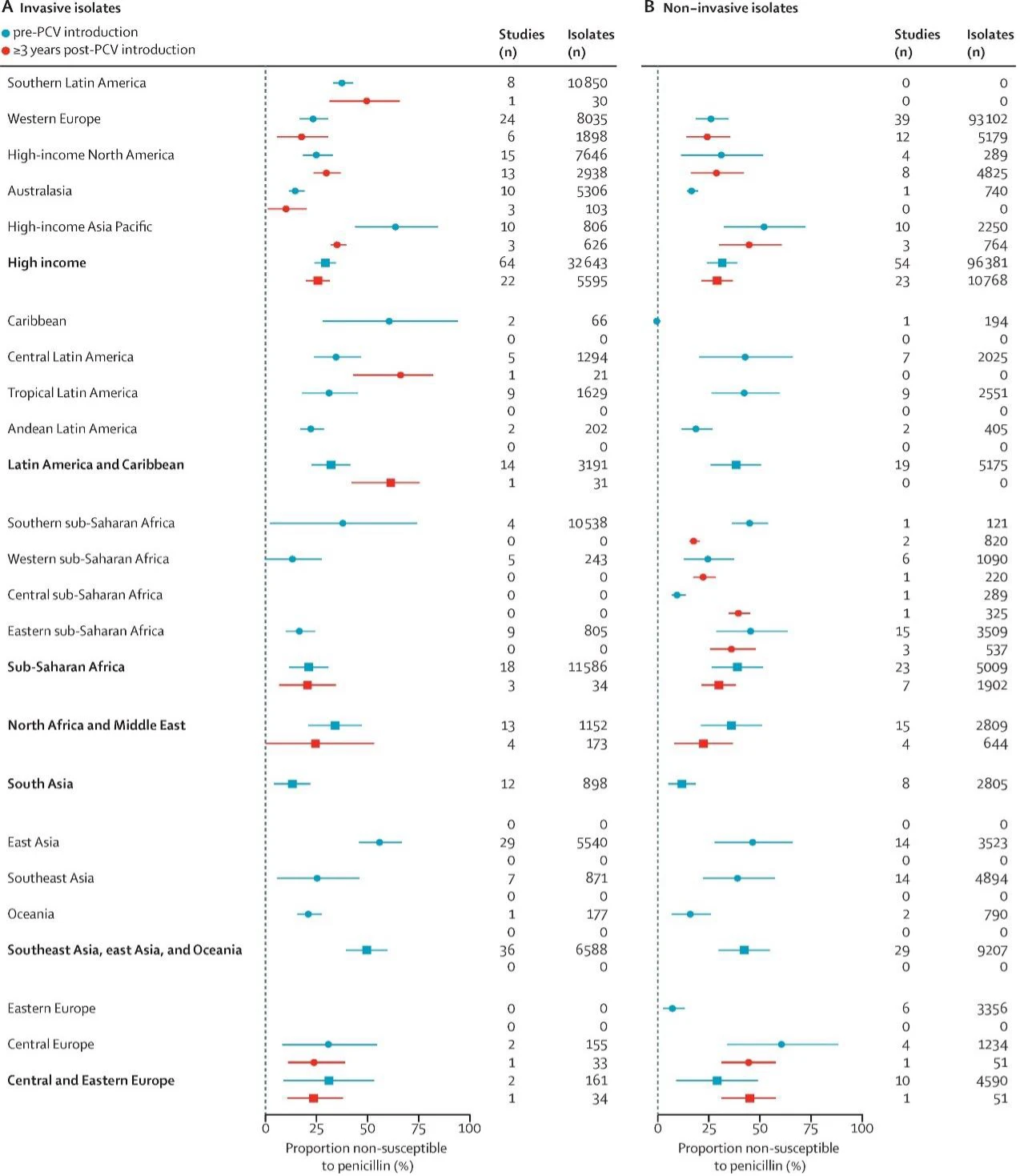
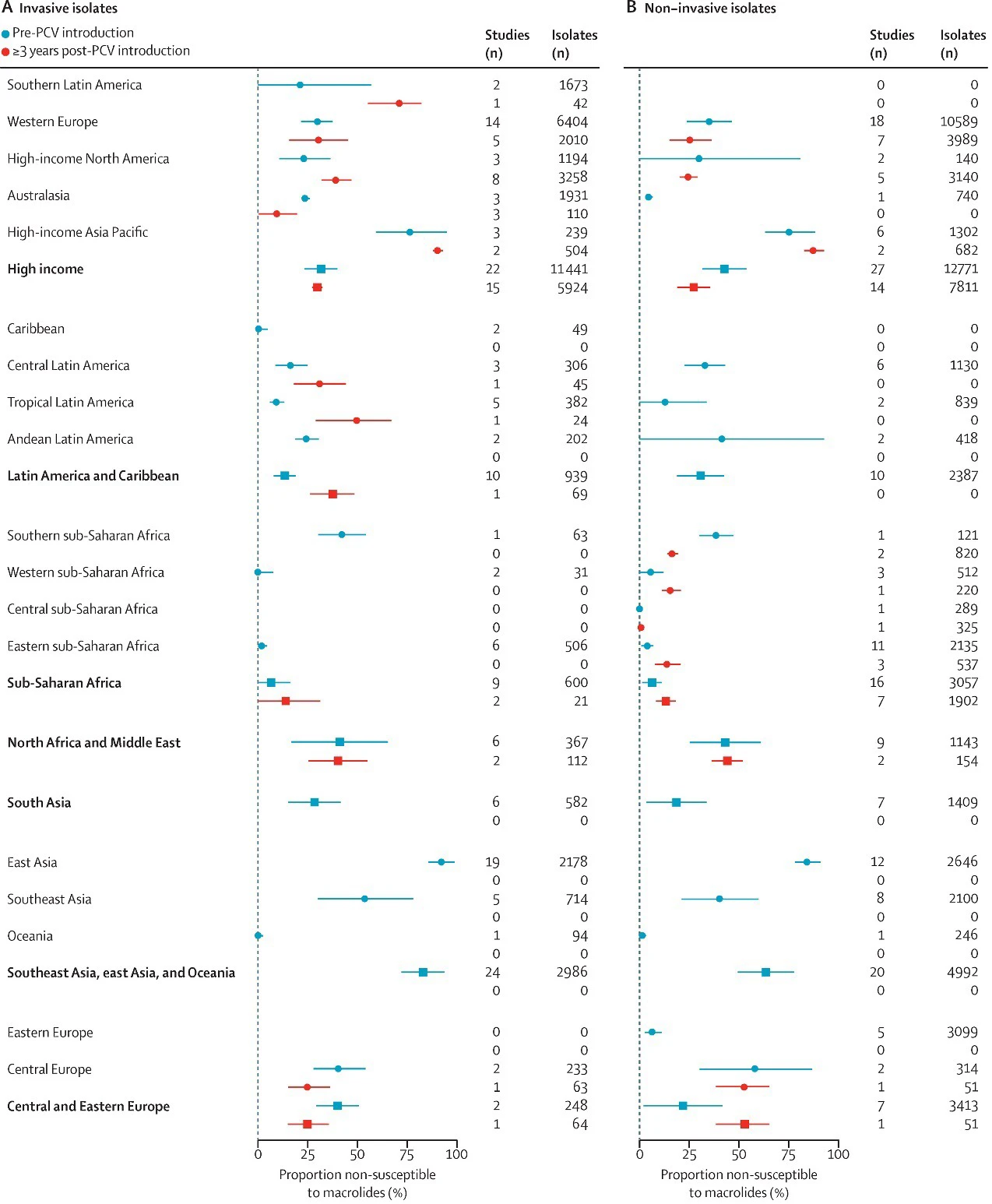
In terms of antimicrobial resistance, a systematic review analyzing the antimicrobial resistance of pediatric Streptococcus pneumoniae isolates demonstrated a decline in non-susceptibility and resistance of penicillin, sulfamethoxazole-trimethoprim, and third-generation cephalosporins following the introduction of the pneumococcal conjugate vaccine (PCV).3 However, resistance to penicillin, macrolides, third-generation cephalosporins, and tetracyclines was highest in Southeast Asia, East Asia, and Oceania. Non-susceptibility of pneumococcal isolates to penicillin in South Asia, East Asia, and high-income Asia-Pacific countries were 13.1% (95% CI: 4.3–21.9%), 56.3% (95% CI: 45.7–66.9%), and 64.2% (95% CI: 43.8–84.4%), respectively (Figures 2 and 3). The point estimates indicated that the resistance of colonizing strains exhibited higher penicillin resistance than that of invasive Streptococcus pneumoniae strains.3
Streptococcus pneumoniae
A study indicates that there were 8.91 million cases of pneumococcal pneumonia among children under the age of 5 worldwide, with 257,000 deaths, resulting in an incidence rate of 1356 per 100,000 and a mortality rate of 36 per 100,000, with a fatality rate of 3% in 2015 (Table 3).4
A systematic review found that the risk of children with non-severe pneumonia developed at least one long-term severe sequela is 5.5%.5 For those with severe pneumonia, the risk is up to 13.6%.5 Furthermore, community-acquired pneumonia (CAP) can lead to cardiac complications. Another systematic review study indicates that among patients with CAP, the incidence rates of heart disease ranges from 2.3% to 17.7%, the rate of acute heart failure ranges from 1.4% to 23.9%, the rate of acute coronary syndrome ranges from 0.1% to 5.3%, and the rate of sudden arrhythmia ranges from 0.9% to 18.5%.6
A global study on the incidence and mortality of pneumonia in children under the age of 5 between 2000 and 2015 showed that, in 2015, 54% of pneumonia and severe pneumonia cases worldwide originated from five developing countries: India, Nigeria, Indonesia, Pakistan, and China in 2015. Compared to 2000, 75% (99 out of 132) of developing countries experienced a reduction of at least 25% in the clinical pneumonia incidence and severe pneumonia, with the most significant decrease observed in China, approximately 69% (Figure 4).2
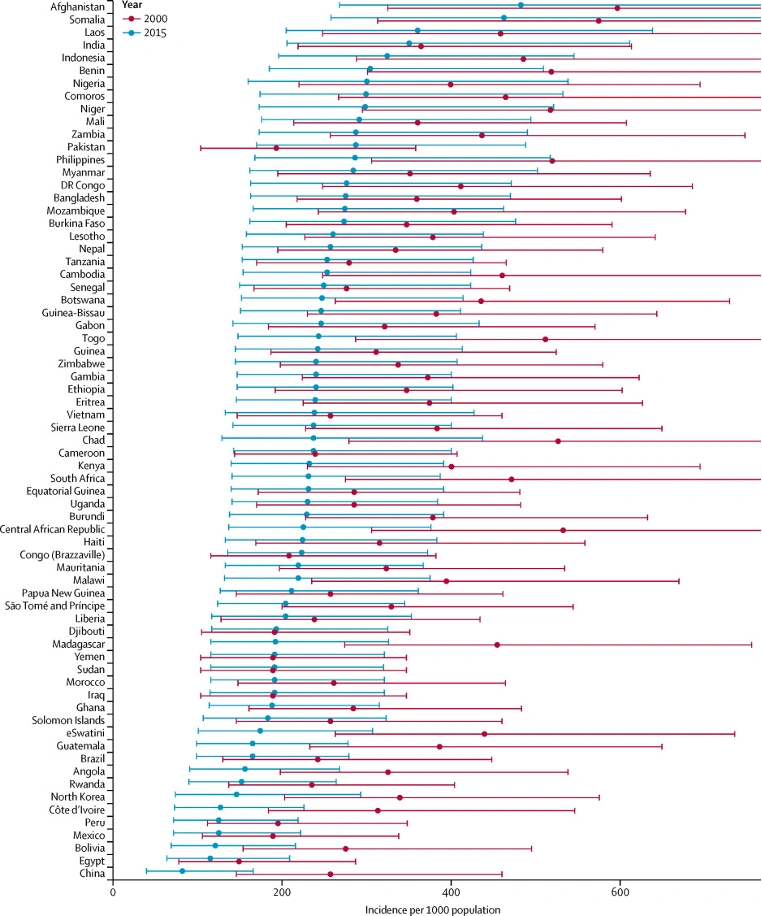
Source:McAllister DA, Liu L, Shi T, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health. 2019;7(1): e47-e57. doi:10.1016/S2214-109X(18)30408-X
Streptococcus pneumoniae meningitis
In 2015, the global pneumococcal meningitis case number in children under 5 years of age was 83,900 and 37,900 deaths, with an incidence rate of 13/100,000, a mortality rate of 5/100,000, and a case-fatality rate of 44% (Table 3).4
A systematic review study shows that the median incidence of post-discharge sequelae among global pneumococcal meningitis cases was 34.7%, with the median incidence rate of at least one mild sequela being 18.6%, and at least one severe sequelae being 24.7%.7 In another systematic review focus on the risk of sequelae from pneumococcal meningitis in high-income countries, it shows that 31.7% of pneumococcal meningitis patients developed sequelae. The respective prevalence rates of hearing loss, seizures, hydrocephalus, spasticity/paralysis, cranial nerve palsy, and visual impairment were 20.9%, 6.5%, 6.8%, 8.7%, 12.2%, and 2.4, respectively.8
Table 3 Morbidity and mortality from Streptococcus pneumoniae disease, global regions, 2015
| the (whole) world | continent | America | Mediterranean region | European | Southeast Asia | the Western pacific region | |||
| Overall situation | |||||||||
| Children aged 1-59 months* | 657,127,399 | 157,167,486 | 73,551,167 | 78,313,066 | 55,681,027 | 175,795,291 | 116,619,363 | ||
| Number of deaths† | 3,260,731 | 1,835,315 | 106,231 | 428,791 | 60,540 | 664,465 | 165,389 | ||
| Deaths due to pneumonia s‡ | 761,193 | 395,431 | 19,560 | 111,895 | 10,453 | 188, 229 | 36,243 | ||
| Deaths due to meningitis‡ | 115,173 | 65,735 | 2,756 | 13,801 | 1,515 | 26,955 | 4,388 | ||
| Disease burden due to Streptococcus pneumoniae | |||||||||
| Morbidity (UR) | 1,419 (1,197-1,737) | 1,603 (1,337-1,997) | 358 (301-441) | 1,261 (1,066-1,542) | 207 (170-261) | 2,509 (2,132-3,048) | 881 (745-1,067) | ||
| Incidence of severe cases (UR) | 559 (411-658) | 619 (452-739) | 142 (104-169) | 491 (362-576) | 129 (94-154) | 986 (729-1154) | 347 (256-404) | ||
| Number of cases (UR) | 9,180,000 (7,870,000-11,400,000) | 2,440,000 (2,100,000-3,140,000) | 259,000 (221,000-325,000) | 968,000 (835,000-1,210,000) | 111,000 (94,800-145,000) | 4,400,000 (3,750,000-5,360,000) | 1,010,000 (868,000-1,240,000) | ||
| Number of serious cases (UR) | 3,670,000 (2,700,000-4,320,000) | 973,000 (710,000-1,160,000) | 104,000 (76,300-124,000) | 385,000 (284,000-451,000) | 72,100 (52,600-85,800) | 1730,000 (1,280,000-2,030,000) | 404,000 (298,000-472,000) | ||
| Mortality rate (UR) | 45 (29-56) | 92 (60-114) | 8 (5-10) | 47 (31-57) | 9 (6-11) | 50 (32-62) | 13 (9-16) | ||
| Deaths (UR) | 318,000 (207,000-395,000) | 166,000 (109,000-205,000) | 5,700 (3,600-7,800) | 37,100 (24,300-45,300) | 4,900 (3,100-6,100) | 88,500 (57,200-111,000) | 15,300 (10,100-18,700) | ||
| Number of deaths of HIV-uninfected children (UR) | 294,000 (192,000-366,000) | 145,000 (94,500-179,000) | 5,700 (3,500-7,700) | 36,700 (24,100-44,800) | 4,800 (3,100-6,100) | 87,200 (56,400-110,000) | 15,200 (10,000-18,600) | ||
| Number of deaths of HIV-infected children (UR) | 23,300 (15,300-28,700) | 21,400 (14,100-26,300) | <100 | 400 (200-500) | <100 | 1,300 (800-1,600) | <100 | ||
| pneumococcal pneumonia | |||||||||
| Morbidity (UR) | 1,356 (1,170-1,612) | 1,504 (1,298-1,788) | 342 (295-406) | 1,214 (1,047-1,443) | 187 (161-222) | 2,432 (2,098-2,891) | 831 (717-987) | ||
| Incidence of severe cases (UR) | 535 (401-609) | 585 (438-667) | 135 (101-154) | 475 (356-541) | 121 (91-138) | 954 (715-1,089) | 326 (244-372) | ||
| Number of cases (UR) | 8,910,000 (7,690,000-10,600,000) | 2,360,000 (2,040,000-2,810,000) | 251,000 (217,000-299,000) | 951,000 (820,000-1,130,000) | 104,000 (89,600-123,000) | 4,280,000 (3,690,000-5,080,000) | 969,000 (836,000-1,150,000) | ||
| Number of serious cases (UR) | 3,520,700 (2,640,000-4,010,000) | 919,000 (689,000-1,050,000) | 99,400 (74,500-113,000) | 372,000 (278,000-424,000) | 67,300 (50,400-76,800) | 1,680,000 (1,260,000-1,910,000) | 380,000 (285,000-433,000) | ||
| Morbidity and mortality rate (UR) | 3% (2-3) | 6% (4-6) | 2% (1-2) | 3% (2-3) | 4% (3-4) | 2% (1-2) | 1% (1-1) | ||
| Severe case fatality rate (UR) | 7% (5-7) | 15% (11-15) | 5% (3-5) | 8% (6-9) | 6% (4-6) | 4% (3-4) | 3% (2-3) | ||
| Mortality rate (UR) | 36 (26-38) | 76 (54-79) | 6 (4-6) | 39 (28-41) | 7 (5-7) | 39 (28-40) | 10 (7-10) | ||
| Deaths (UR) | 257,000 (182,000-268,000) | 137,000 (96,900-142,000) | 4,600 (3,200-4,800) | 31,000 (22,000-32,300) | 3,800 (2,700-4,000) | 69,200 (49,100-72,100) | 11,600 (8,200-12,100) | ||
| Number of deaths of HIV-uninfected children (UR) | 238,000 (169,000-248,000) | 119,000 (84,300-124,000) | 4,500 (3,200-4,700) | 30,700 (21,800-32,000) | 3,800 (2,700-4,000) | 68,200 (48,400-71,100) | 11,600 (8,200-12,000) | ||
| Number of deaths of HIV-infected children (UR) | 19,300 (13,700-20,100) | 17,800 (12,600-18,600) | <100 | 300 (200-300) | <100 | 1,000 (700-1,000) | <100 | ||
| pneumococcal meningitis | |||||||||
| Morbidity (UR) | 13 (5-26) | 21 (9-45) | 3 (1-7) | 10 (4-21) | 4 (2-8) | 15 (6-31) | 10 (5-15) | ||
| Number of cases (UR) | 83,900 (36,100-169,000) | 29,400 (11,800-62,300) | 2,300 (900-5,000) | 7,900 (3,200-16,500) | 2,200 (1,000-4,200) | 26,100 (11,200-52,900) | 11,400 (6,300-18,000) | ||
| Morbidity and mortality rate (UR) | 44% (18-93) | 61% (24-100) | 27% (8-70) | 52% (21-100) | 25% (10-50) | 39% (16-79) | 17% (8-30) | ||
| Mortality rate (UR) | 5 (2-11) | 13 (5-28) | 1 (0-2) | 5 (2-11) | 1 (0-2) | 6 (2-12) | 2 (1-3) | ||
| Deaths (UR) | 37,900 (15,400-79,700) | 20,400 (8,000-43,700) | 600 (200-1,600) | 4,200 (1,600-8,900) | 600 (200-1,100) | 10,200 (4,300-20,800) | 1,900 (1,000-3,500) | ||
| Number of deaths of HIV-uninfected children (UR) | 35,200 (14,300-73,800) | 17,900 (7,000-38,300) | 600 (200-1,600) | 4,100 (1,600-8,800) | 550 (200-1,100) | 10,100 (4,300-20,500) | 1,900 (1,000-3,500) | ||
| Number of deaths of HIV-infected children (UR) | 2,700 (1,100-5,900) | 2,500 (1,000-5,400) | <100 | <100 | <100 | 200 (100-300) | <100 | ||
| Non-pneumonia non-meningitis pneumococcal disease | |||||||||
| Morbidity (UR) | 50 (22-100) | 77 (31-164) | 13 (5-28) | 37 (15-78) | 17 (7-32) | 62 (27-127) | 41 (22-64) | ||
| Incidence of severe cases (UR) | 11 (5-22) | 13 (5-27) | 4 (1-8) | 6 (2-13) | 5 (2-9) | 17 (7-35) | 11 (6-18) | ||
| Incidence of non-serious cases (UR) | 39 (17-78) | 64 (26-137) | 9 (4-21) | 31 (12-64) | 12 (5-23) | 45 (19-92) | 30 (16-47) | ||
| Number of cases (UR) | 326,000 (142,000-653,000) | 122,000 (49,000-257,000) | 9,500 (3,600-21,000) | 29,000 (12,000-60,900) | 9,300 (4,200-18,000) | 110,000 (47,100-223,000) | 47,500 (26,000-75,000) | ||
| Number of serious cases (UR) | 73,400 (32,400-145,000) | 20,500 (8,400-42,800) | 2,600 (1,000-5,700) | 4,900 (1,900-10,400) | 2,500 (1,100-4,800) | 29,900 (12,800-60,700) | 13,000 (7,100-20,500) | ||
| Number of non-serious cases (UR) | 253,000 (109,000-510,000) | 101,000 (41,000-215,000) | 6,900 (2,600-15,000) | 24,000 (9,600-50,500) | 6,700 (3,000-13,000) | 79,900 (34,300-162,000) | 34,500 (19,000-54,500) | ||
| Morbidity and mortality (UR)§ | 31% (13-63) | 44% (17-94) | 21% (6-55) | 38% (14-82) | 19% (8-39) | 30% (13-62) | 13% (7-24) | ||
| Mortality rate (UR) | 3 (1-7) | 5 (2-11) | 1 (0-2) | 2 (1-5) | 1 (0-2) | 5 (2-10) | 1 (1-3) | ||
| Deaths (UR) | 22,700 (9,400-47,200) | 9,000 (3,600-19,100) | 600 (200-1,400) | 1,900 (700-4,100) | 500 (200-1,000) | 9,100 (3,800-18,400) | 1,700 (900-3,100) | ||
| Number of deaths of HIV-uninfected children (UR) | 21,500 (8,800-44,500) | 7,900 (3,100-16,800) | 600 (200-1,400) | 1,900 (700-4,000) | 500 (200-1,000) | 8,900 (3,800-18,100) | 1,700 (900-3,100) | ||
| Number of deaths of HIV-infected children (UR) | 1,300 (500-2,700) | 1,100 (400-2,300) | <100 | <100 | <100 | 100 (100-300) | <100 | ||
Note: Data are estimates (UR=uncertainty range). Mortality and morbidity rates are in units per 100,000 children. Morbidity and morbidity estimates include all children, regardless of whether they are HIV-infected or not, and mortality and death estimates exclude HIV-infected children unless otherwise noted.
*Data derived from the United Nations World Population Prospects 2015.
†Data from the United Nations Child Mortality Assessment 2015.
‡Data from Maternal and Child Epidemiological Estimates/World Health Organization joint estimates
§For children with severe non-pneumonia non-meningitis only
Streptococcus pneumoniae bacteraemia
A systematic review in Latin America showed that 8% (95% CI: 5.3-12.4) of 1,218 cases of pneumococcal disease were Streptococcus pneumoniae bacteremia. The incidence of Streptococcus pneumoniae bacteremia was 3.9 per 100,000 among children under five, and 5.8 per 100,000 among children under two.9 According to a study in Chile, most cases occur in the fall and winter season, with an in-hospital mortality rate of 33.3%.10
A systematic review found that 16 (1.5%) of 1,062 patients with invasive pneumococcal disease developed arthritis. Furthermore, bacteremia occurred in 69% of patients with primary septic arthritis and in 80% of patients with prosthetic joint infections. The morbidity and mortality of pneumococcal arthritis varied, with case fatality rates reported as high as 32%. 11
Content Editor: Menglu Jiang, Ziqi Liu
Page Editor: Ziqi Liu
References
- Rudan I, Boschi-Pinto C, Biloglav Z, et al. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86(5):408-416.
- McAllister DA, Liu L, Shi T, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health. 2019;7(1): e47-e57. doi:10.1016/S2214-109X(18)30408-X
- Andrejko K, Ratnasiri B, Hausdorff WP, et al. Antimicrobial resistance in paediatric Streptococcus pneumoniae isolates amid global implementation of pneumococcal conjugate vaccines: a systematic review and meta-regression analysis. Lancet Microbe. 2021 Sep;2(9): e450-e460.
- Wahl, B., O’Brien, K. L., Greenbaum, A, et al. (2018). Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000-15. The Lancet. Global health, 6(7), e744–e757. https://doi.org/10.1016/S2214-109X(18)30247-X
- Walker CLF, Rudan I, Liu L, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013 Apr 20;381(9875):1405-1416.
- Corrales-Medina VF, Suh KN, Rose G, et al. Cardiac complications in patients with community-acquired pneumonia: a systematic review and meta-analysis of observational studies. PLoS Med. 2011 Jun;8(6):e1001048.
- McAllister DA, Liu L, Shi T, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health. 2019 Jan;7(1):e47-e57.
- Edmond K, Clark A, Korczak VS, et al. Global and regional risk of disabling sequelae from bacterial meningitis: a systematic review and meta-analysis. Lancet Infect Dis. 2010 May;10(5):317-28.
- Jit M. The risk of sequelae due to pneumococcal meningitis in high-income countries: a systematic review and meta-analysis. J Infect. 2010 Jul;61(2):114-24.
- Ciapponi A, Elorriaga N, Rojas JI, et al.Epidemiology of pediatric pneumococcal meningitis and bacteremia in Latin America and the Caribbean: a systematic review and meta-analysis. Pediatr Infect Dis J. 2014 Sep;33(9):971-8.
- Fica A, Bunster N, Aliaga F, et al. Bacteremic pneumococcal pneumonia: serotype distribution, antimicrobial susceptibility, severity scores, risk factors, and mortality in a single center in Chile. Braz J Infect Dis. 2014 Mar-Apr;18(2):115-23.
- Dernoncourt A, El Samad Y, Schmidt J, et al. Case Studies and Literature Review of Pneumococcal Septic Arthritis in Adults. Emerg Infect Dis. 2019 Oct;25(10):1824–33.





